Dr. O'Donoghue's Publications
Dr. O'Donoghue occasionally writes or co-authors articles for contribution to outstanding publications including "Cosmetic Dermatology", "Cutis", “Journal of American Academy of Dermatology” and the “Journal on Dermatology Research”.
Below are some of the more recent articles - please click on the "read more" button to view the entire article.
To view a PDF Version of the following articles - please click on the following links:
- Ulcerative Lichen Planus with an Unusual Lichenoid Infiltrate Masquerading as Secondary Syphilis (Kevin A O'Donoghue, J Morgan O'Donoghue, Samantha A Marrone, Vincenzo Giannelli, Elizabeth Dugan) Journal of Dermatology Research 01/19/2026
- A Unique and Economical Technique for Reducing Pathogen Exposure During Dermatologic Surgical Procedures (Kevin Andrew O’Donoghue, J Morgan O’Donoghue) - Journal of Dermatology Research 10/27/2025
- Erosive lichen planus with an unusual plasma cell infiltrate masquerading as secondary syphilis - submitted to Cutis
- Bilateral Subcutaneous Island Pedicle Flap for Lower Extremity Surgical Defects - Cosmetic Dermatology October 2008 Volume 21 No.10
- Novel Use of a Pressure Bandage for Assistance During Surgery - Cosmetic Dermatology April 2009 Volume 22 No. 4
- The use of skin biopsies to assess response to systemic corticosteroid therapy in early stage toxic epidermal necrolysis - Cutis 2009;84:138-140,161-162
- Extensive Erythema Multiforme With an Unusual Delineated Presentation: A Case Report - Cosmetic Dermatology May 2011 Vol 24 No. 5
- A Novel Method of Mohs Defect Closure Using Posterior Deltoid Skin - (JAAD Online Surgical pearl) Journal of the American Academy of Dermatology - Reprinted Volume 84, Issue 4, April 2021
A Novel Method of Mohs Defect Closure Using Posterior Deltoid Skin
Journal of the American Academy of Dermatology (JAAD) 2021 Apr;84(4):e191-e192.
doi: 10.1016/j.jaad.2019.09.076. Epub 2019 Oct 8.
SURGICAL CHALLENGE
Patients who undergo Mohs surgery may be left with sizeable defects and require skin grafts. Repair may prove especially challenging when the surgeon is faced with a large defect in a patient who is elderly with fragile, atrophic skin. Traditional donor sites for harvesting grafts can be difficult for patients to care for, heal slowly, and result in poor cosmesis.
SOLUTION
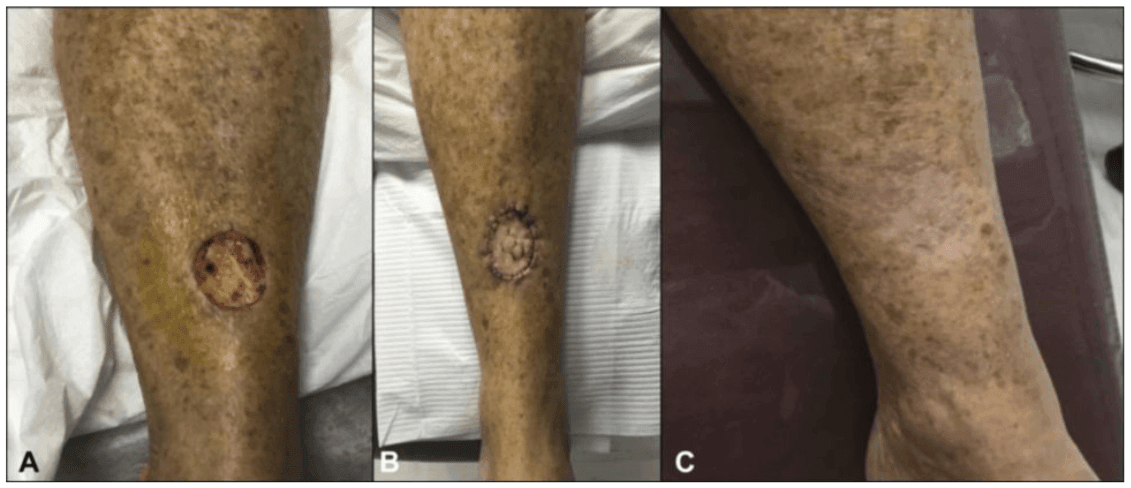
Mohs surgery of the lower tibia resulted in a 3 34-cm defect (Fig 1, A). A graft was determined to be the best closure option. The upper lateral arm was chosen as the donor site; this location provides an accessible area for the patient to care for and, when healed, often resembles the scar that commonly results from smallpox vaccinations (Fig 2).
Fig 1. A, Lower tibial defect. B, Graft sutured in place. C, Healed lower tibial graft site.

The donor site on the upper deltoid is marked and anesthetized. A flexible disposable blade is coated with petrolatum, and graft excision is performed using delicate, side-to-side movements. The flexible blade allows precise control of the diameter, thickness, and beveled peripheral graft edge. The size of this donor tissue should be approximately 10% larger than the defect to account for normal tissue contraction. The graft is then gently trimmed and secured in the defect with interrupted 6.0 nylon sutures. Several 2-mm slits are placed in the graft to allow for exudative drainage, and a bolster is applied (Fig 1, B). This surgical technique illustrates the benefits of the posterior upper arm as a donor site, ease of use, quick healing, and excellent cosmesis (Fig 1, C).
We thank Dr S. Mark Burnett for sharing this interesting surgical technique.
Novel use of a pressure bandage for assistance during surgery
Cosmetic Dermatology April 2009 Volume 22 No. 4
The ability to perform surgery efficently and safely is a necessity to the dermatologic surgeon.
Sometimes, depending on various situations, the dermatologist may find themselves doing surgery without the luxury of an assistant. One of the most valuable services a surgical assistant provides is blotting excess blood in the field. We describe a novel technique for the dermatologic surgeon to use to provide temporary blotting and collection of blood when a surgical assistant is not readily available.
Technique:
In our clinic multiple small surgical procedures are performed daily. These wounds are often dressed with a sterile 3x3 4 ply cotton ultra-gauze by crosstex covered by Hypafix Conformable Retention Tape. Hypafix is a low allergy adhesive, non woven dressing retention sheet. Hypafix is easily conformable, increasing adhesion to a variety of body parts, while allowing freedom of movement. It comes in a broad size range to give complete coverage of any wound. Hypafix is indicated for post-operative wound dressing, gauze retention, securing catheter and drainage tubes, and patello-femoral positioning techniques.
We suggest a novel use for the Hypafix dressing which will allow the dermatologist freedom to perform surgical procedures solo. We suggest leaving Hypafix attached at the base, in a gravitationally dependent position. (Fig 1) It can then function to catch any blood or debris that might drip from your surgical field. (Fig 2) This same dressing can then be reused after the procedure to cover the wound site. This simple technique can save time for the dermatologist as well as provide a successful way to perform surgery without an assistant.
Extensive Erythema Multiforme With an Unusual Delineated Presentation: A Case Report
COSMETIC DERMATOLOGY MAY 2011 VOL 24 NO. 5
J Morgan O'Donoghue, MD and Kate Ross, MD
Dr J Morgan O'Donoghue is the medical director of O'Donoghue Dermatology in Sarasota, Florida, Kate Ross, MD is with the University of South Florida Department of Dermatology. The authors report no conflict of interest in relation to this article. Correspondence: J Morgan O'Donoghue, MD, 1952 Field Road Sarasota, Florida 34231
Erythema Multiforme majus (EMM) is a hypersensitivity reaction usually secondary to medications, viruses or other infections. Its presentation is fairly typical with a symmetrical distribution of vesicles, bullae or tagetoid lesions on the upper body arms, legs, palms, feet and oral mucosa. The authors present a case of EMM with a very unusual clinical presentation evolving over time into a unique, almost dermatomal distribution. Typical therapies were not initially helpful and intravenous antibody had to be administered.
Erythema multiforme majus (EMM), Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN) were once believed to be on a spectrum of severe cutaneous adverse reactions. In the past few years, it has been debated that EMM is, in fact, a separate entity from SJS and TEN.1
Auquier-Dunant et al1 reported that EMM occurs most often in young male individuals, with a 10-fold higher rate of recurrence and a milder presentation than are found in patients with SJS or TEN. Herpes has been identified as the principal risk factor, occurring in 70% to 80% of cases of EMM.2 Multiple target lesions are present, affecting less than 10% of the body surface area (BSA). It is often symmetric, with the distribution beginning acrally (dorsal surfaces of hands, feet, elbows, and knees).3 Oral lesions are found in 70% of cases but are not required for diagnosis.3
The Use Of Skin Biopsies To Assess Response To Systemic Corticosteroid Therapy In Early Stage Toxic Epidermal Necrolysis
Cutis 2009;84:138-140,161-162
Report of a case and review of the literature
J Morgan O’Donoghue, MD - Yvana P. Céspedes, MD - Paul F. Rockley, MD - Thomas P. Nigra, MD
CASE REPORT
A 26-year-old white female with a past medical history remarkable for systemic lupus erythematosus and vasculitis developed grand mal seizures, which were controlled with oral phenytoin 300 milligrams per day. Three weeks later, she noticed the onset of generalized pruritus and skin tenderness. The following day, she developed fever, chills, mucous membrane swelling and a symmetrical, erythematous, morbilliform eruption on the extensor aspects of the distal extremities. During the next 24 hours, the eruption slowly evolved from discrete, reddish macules and papules to confluent, necrotic blisters involving the extremities, trunk, head, neck, and mucosal surfaces
At the time of examination the patient had a temperature of 40 C, widespread tender erythema, hemorrhagic vesiculobullous lesions and seropurulent, crusted erosions. Approximately 20 percent of the body surface area was covered with necrotic epidermis. A positive direct Nikolsky sign was noted on lesional skin only. Mucosal surfaces contained some inflammatory bullous and erosive lesions. Conjunctival involvement was characterized by bilateral cheimosis, redness and lacrimation.
Bilateral Subcutaneous Island Pedicle Flap For Closure Of Lower Extremity Surgical Defects.
Cosmetic Dermatology October 2008 Volume 21 No.10
J. Morgan O'Donoghue, MD - Kevin M. Cronin, BA
The closure of some lower extremity surgical defects may challenge the dermatologic surgeon. This is especially the case with older patients who have severely atrophic, friable skin that makes suture placement difficult if there is any wound tension.
We describe the bilateral subcutaneous island pedicle flap as a suitable closure technique for lower extremity defects when primary linear or layered closure is not an option. In our case report, 2 triangular flaps on opposite sides of the defect were incised down to the subcutaneous tissue, advanced into the surgical defect, and sutured into place with buried subcutaneous sutures.
This repair is an excellent consideration for thin skin resembling tissue paper in which minimal wound tension is necessary for sutures to hold properly. The bilateral subcutaneous island pedicle flap is a versatile, effective means of repairing many lower extremity defects when primary linear or layered closure is not an option.
A variety of repairs has been described for closure of surgical lower extremity defects. These include second intention, full- and split-thickness skin grafts, rotation flaps, triangular flaps, and primary closures, side¬to-side layered closures, or simple closures. The bilateral sub¬cutaneous island pedicle flap, or bilateral V -Y advancement flap, is shown to be a versatile, effective means of repairing many facial defects following excisional surgery and has been widely described for defects of the ear, nasolabial fold, and lip area. We demonstrate how this repair may also be considered for closure of lower extremity defects.